Some frequently asked questions...
What is a colonoscopy?
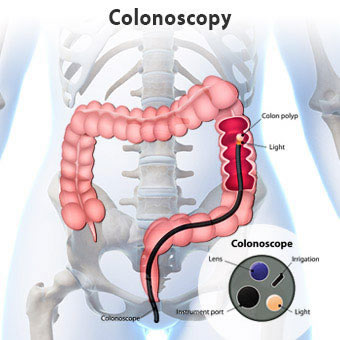
A colonoscopy is a procedure that enables your specialist doctor to carefully examine the lining of the colon (also called the large bowel or large intestine). It is used for diagnosing and treating a variety of problems encountered in the colon or large bowel.
Why is a colonoscopy performed?
We follow national guidelines. You may need a colonoscopy:
- as part of routine screening for cancer (family history guidelines)
- on patients with known polyps or previous polyp removal (surveillance guidelines)
- follow up after bowel cancer (surveillance guidelines)
- to evaluate new bowel symptoms which could include blood and/or mucous in the bowel motion, persistent abdominal pain or discomfort, or change in bowel habit.
- to evaluate chronic diseases such as inflammatory disorders (Crohn's or ulcerative colitis).
What preparation is required in advance of the colonoscopy?
It is very important that your bowel is thoroughly emptied so that the lining can be clearly seen. You will need to stop eating some foods for several days before your colonoscopy. You will also need to drink a special bowel cleansing preparation (Glycoprep-C) which will make you go to the toilet several times. Separate instructions on diet and bowel preparation will be sent to you by Kensington Hospital. It is important you follow these instructions to ensure optimal visualisation of your colon by the specialist undertaking your colonoscopy. Your specialist may abandon or need to repeat the procedure if stools are still seen in the bowel.
Please take your normal medication with a small amount of water.
If you are taking blood thinning medication such as Warfarin, Ticagrelor (Brilinta), Clopidogrel (Plavix), Dabigatran (Pradaxa) or oral iron tablets, please contact your specialist’s rooms as they may need to be stopped 3-5 days prior to your appointment. Please contact your specialist’s room a minimum of a week prior to your appointment.
Please bring a list of any medications you are currently taking to Kensington Hospital. It is important you bring with you any inhalers, angina sprays and diabetic medication.
You will need someone to bring you to the hospital and to take you home after your colonoscopy. YOU CANNOT DRIVE YOURSELF because you will have been given some medication to make you sleepy (sedation).
What can be expected during the colonoscopy?
Your specialist will explain the procedure and you will be required to sign a consent form. This confirms that you understand the examination and agree to go ahead. Please ask any questions you may have. It is important that you fully understand what is happening.
The procedure is done with a combination of sedative and pain relief which is often administered by an anaesthetist. This could make you feel drowsy and may cause you to forget the procedure. You may experience some discomfort during the procedure. More pain relief/sedation may be given to a maximum safe dose. A nurse will be with you throughout the procedure. The procedure takes approximately 30 to 45 minutes.
The procedure involves your specialist putting a flexible tube into your anus (bottom) which will be manoeuvred around your lower bowel (colon) and if required possibly into the last part of your small bowel (terminal ileum). There is a small camera on the end of the tube which is used to examine the lining of your bowel, to see if there are any problems.
A small tissue sample may be taken (biopsy) and polyps removed or sampled and sent for testing. If you wish this tissue to be returned for cultural or spiritual reasons you need to let us know before the procedure and be aware this may have been preserved in a toxic chemical (formaldehyde) and be in a plastic container to prevent contamination. If further information is required, do not hesitate to ask.
What if the colonoscopy shows an abnormality?
If your specialist sees an area that needs more detailed evaluation, a biopsy may be obtained and submitted to a laboratory for analysis. Placing a special instrument through the colonoscope to sample the lining of the colon does this. Polyps are generally removed. The majority of polyps are benign (non-cancerous), but your specialist cannot always tell by the appearance alone. They can be removed by burning (fulgurating) or by a wire loop (snare). It may take your specialist more than one sitting to do this if there are numerous polyps or they are very large. Sites of bleeding can be identified and controlled by injecting certain medications or coagulating (burning) the bleeding vessels. Biopsies do not imply cancer, however, removal of a colonic polyp is an important means of preventing colorectal cancer.
What happens after the colonoscopy?
You will return to the hospital recovery area after your colonoscopy. As you have had sedation you will need to rest for 30 minutes. On recovery you can eat and drink as normal.
The nurse or specialist will discuss the result of the examination before you go home and give you a written report. A report will be sent to your GP with the results of any biopsies taken. This may take up to three weeks. You may be required to attend a follow up appointment.
As you have had a sedative you must have a responsible adult to take you home and stay with you for a minimum of six hours. You cannot wait outside for them or catch a taxi or bus alone. You must not drive, drink alcohol, operate machinery or sign important documents for 24 hours after the procedure.
It is important to drink plenty of fluids following the procedure and we recommend a light diet. You may have some abdominal discomfort for a few hours. This is due to air pumped into your colon during the procedure. This can be relieved by soaking in a hot bath, placing a hot pad on your abdomen or taking two Panadol tablets 4—6 hourly (to a maximum of 8 tablets in 24 hours). You may have altered bowel habits for a few days after the procedure.
If polyps were found during your procedure, you may need to have a repeat colonoscopy. Your specialist will decide on the frequency of your colonoscopy exams.
What complications can occur?
Most colonoscopies are safe and uncomplicated. However, as with any procedure there is a small chance of side effects or complications. These range from discomfort and pain during the procedure, bleeding which is usually minor and stops on its own but may require a transfusion or re-intervention, and the small possibility of a perforation (making a hole). This is rare occurring in less than 1:1000 although the risk does go up if interventions are undertaken. This could require an operation with the formation of a stoma (a bag) this may be temporary or permanent and may require removal or repair of part of the bowel. You should also be aware that this examination is not perfect and even with a skilled endoscopist some abnormalities may be missed.
It is important to contact your specialist if you notice symptoms of severe abdominal pain, fevers, chills or rectal bleeding of more than one-half cup. Bleeding can occur up to several days after a biopsy.
What is the difference between a colonoscopy and CT colonography
A CT colonography is a CT scan of your abdomen specifically examining your large bowel or colon. If a cancer or polyp is detected, you may still need to undergo a colonoscopy in order to remove any polyps. If a cancer is found a colonoscopy is needed so that a biopsy of this can be taken.
Who will be there when I have my colonoscopy
Your specialist surgeon or gastroenterologist. There will be an anaesthetist who will give you the sedation and monitor your heart and breathing. It takes a minimum of three trained nursing staff to assist with the procedure. One of these will be helping the anaesthetist and the other two will assist during the colonoscopy to take biopsies, set up the equipment and document the important points of the procedure.